
We are a different kind of PBM.
We negotiate on the same side as our clients.
Alluma is a provider-led, provider-focused Pharmacy Benefits Manager (PBM) that prioritizes patient outcomes over profits. Alluma is committed to transparency, clinical collaboration, and resource optimization.


We partner with our clients to achieve the best outcomes.
We do not own pharmacies.
Alluma aligns incentives across your drug purchasing program, on-site pharmacies, clinical practice, employee health plans, and members, creating a cohesive strategy that maximizes value.

Why choose Alluma?
Provider-led focus
Alluma was developed through a partnership between Vizient and Mayo Clinic, which positions it to prioritize clinical outcomes rather than profits. This focus on patient care and alignment with healthcare providers ensures that health systems and patients benefit more directly from pharmacy services.
Transparency in pricing
Unlike traditional PBMs, Alluma operates with a transparent fee structure. It only charges a management fee and prior authorization fee, avoiding hidden markups and rebates that are common in the industry.
Clinical collaboration
Alluma emphasizes whole-patient care by integrating clinical pharmacy services with health systems. This collaboration ensures that treatment decisions are made based on clinical evidence and patient needs, rather than focusing solely on reducing medication costs.
Pharmacy resource optimization
The Alluma model incentivizes the use of health system-owned or affiliated pharmacies, driving increased prescription capture and improving coordination of care. By aligning incentives and optimizing in-house pharmacy use, Alluma captures more prescriptions, improves care coordination and generates more revenue.
Advanced analytics and insights
Alluma provides robust data analytics and clinical insights, giving healthcare systems visibility into their pharmacy spend and enabling them to make informed decisions that optimize both costs and health outcomes.
Dedicated account team
We’re dedicated to supporting your health system from start to finish. Our team of experienced account managers and pharmacists will work directly with you and on a consistent basis to keep you on track.
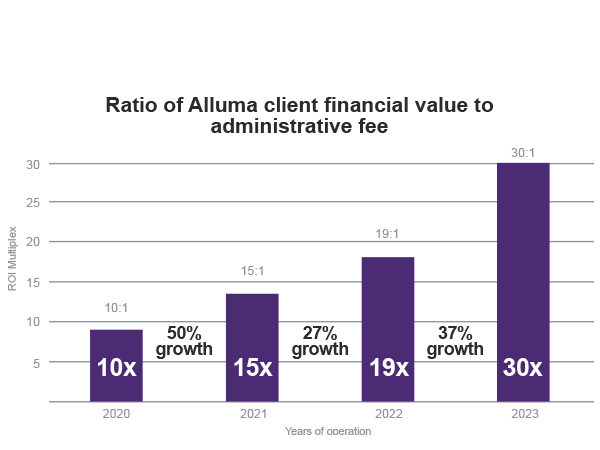
Alluma model continues to support client growth
100% pass-through of rebates and savings
- Alluma provides 100% pass-through of rebates and savings: 30:1 Return on Admin Fee in 2023
- Alluma members have consistently shown 15% higher formulary compliance relative to the Employer-Hospital Benchmark, which contributes to above-market savings
- With the Alluma model, on average, 49% of claims were captured, equating to 51% of revenue.
Stay informed
Sign up for email updates and get the latest news, industry trends and expert tips delivered straight to your inbox. Be the first to learn how we’re transforming pharmacy benefits and helping organizations like yours achieve better health outcomes.